Important Safety Information
Contraindications
- Patients with known or suspected gastrointestinal (GI) obstruction and patients at increased
risk of recurrent obstruction, due to the potential for GI perforation.
- Patients with a history of a hypersensitivity reaction to Symproic® (naldemedine). Reactions have included
bronchospasm and rash.
Warnings and Precautions
Cases of GI perforation have been reported with use of another peripherally acting opioid antagonist
in patients with conditions that may be associated with localized or diffuse reduction of structural
integrity in the wall of the GI tract. Monitor for the development of severe, persistent, or
worsening abdominal pain; discontinue if this symptom develops.
Symptoms consistent with opioid withdrawal, including hyperhidrosis, chills, increased lacrimation,
hot flush/flushing, pyrexia, sneezing, feeling cold, abdominal pain, diarrhea, nausea, and vomiting
have occurred in patients treated with Symproic.
Patients having disruptions to the blood-brain barrier may be at increased risk for opioid withdrawal
or reduced analgesia. Take into account the overall risk-benefit profile when using Symproic in such
patients. Monitor for symptoms of opioid withdrawal in such patients.
Drug Interactions
Avoid use with strong CYP3A inducers (e.g., rifampin) because they may reduce the efficacy of Symproic.
Use with moderate (e.g., fluconazole) and strong (e.g., itraconazole) CYP3A inhibitors and
P-glycoprotein inhibitors (e.g., cyclosporine) may increase Symproic concentrations. Monitor for
potential adverse reactions.
Avoid use of Symproic with another opioid antagonist due to potential for additive effect and
increased risk of opioid withdrawal.
Use in Specific Populations
Symproic crosses the placenta and may precipitate opioid withdrawal in a fetus due to the immature
fetal blood-brain barrier. Symproic should be used during pregnancy only if the potential benefit
justifies the potential risk. Because of the potential for serious adverse reactions, including
opioid withdrawal in breastfed infants, a decision should be made to discontinue breastfeeding or
discontinue the drug, taking into account the importance of the drug to the mother.
Avoid use in patients with severe hepatic impairment. No dose adjustment of Symproic is required in
patients with mild or moderate hepatic impairment.
Adverse Reactions
The most common adverse reactions with Symproic as compared to placebo in clinical trials were: abdominal pain (8% vs 2%), diarrhea (7% vs 2%), nausea (4% vs 2%), and gastroenteritis (2% vs
1%).
In pooled Studies 1 and 2, the incidence of adverse reactions of opioid withdrawal was 1% (8/542) for
Symproic and 1% (3/546) for placebo. In Study 3 (52-week data), the incidence was 3% (20/621) for
Symproic and 1% (9/619) for placebo.
To report suspected Adverse Reactions, contact Shionogi at 1‑800‑849‑9707 or FDA at 1‑800‑FDA‑1088 or
www.fda.gov/medwatch.
Indication
Symproic is indicated for the treatment of opioid-induced constipation (OIC) in adult patients with chronic
non-cancer pain, including patients with chronic pain related to prior cancer or its treatment who do not require frequent
(e.g., weekly) opioid dosage escalation.
Please see Full
Prescribing Information and Medication Guide for Symproic.
References: 1. Argoff CE, Brennan MJ, Camilleri M, et al. Consensus recommendations on
initiating prescription therapies for opioid-induced constipation. Pain Med.
2015;16(12):2324-2337. 2. Kalso E, Edwards JE, Moore RA, McQuay HJ. Opioids in chronic
non-cancer pain: systematic review of efficacy and safety. Pain. 2004;112(3):372-380. 3. Cook
SF, Lanza L, Zhou X, et al. Gastrointestinal side effects in chronic opioid users: results from
a population-based survey. Aliment Pharmacol Ther. 2008;27(12):1224-1232. 4. Brown RT,
Zuelsdorff M, Fleming M. Adverse effects and cognitive function among primary care patients
taking opioids for chronic nonmalignant pain. J Opioid Manag. 2006;2(3):137-146. 5. Tuteja AK,
Biskupiak J, Stoddard GJ, Lipman AG. Opioid-induced bowel disorders and narcotic bowel syndrome
in patients with chronic non-cancer pain. Neurogastroenterol Motil. 2010;22(4):424-e96. 6. Coyne
KS, LoCasale RJ, Datto CJ, Sexton CC, Yeomans K, Tack J. Opioid-induced constipation in patients
with chronic noncancer pain in the USA, Canada, Germany, and the UK: descriptive analysis of
baseline patient-reported outcomes and retrospective chart review. Clinicoecon Outcomes Res.
2014;6:269-281. 7. Emmanuel A, Johnson M, McSkimming P, Dickerson S. Laxatives do not improve
symptoms of opioid-induced constipation: results of a patient survey Pain Med. 2017;18(10):1932-1940. doi:10.1093/pm/pnw240 8. Camilleri M, Drossman DA, Becker G, Webster LR,
Davies AN, Mawe GM. Emerging treatments in neurogastroenterology: a multidisciplinary working
group consensus statement on opioid-induced constipation. Neurogastroenterol Motil.
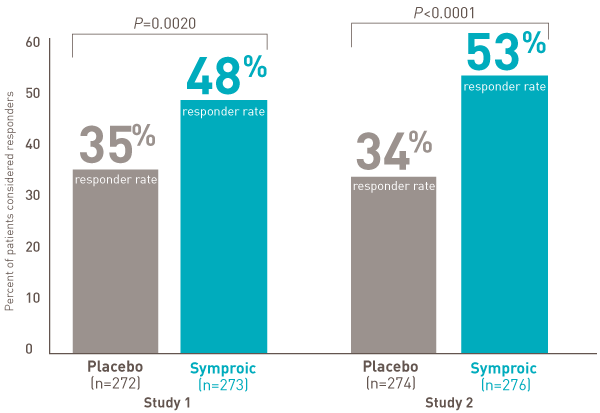
2014;26(10):1386-1395. 9. Hale M, Wild J, Reddy J, Yamada T, Arjona Ferreira JC.
Naldemedine versus placebo for opioid-induced constipation (COMPOSE-1 and COMPOSE-2): two
multicentre, phase 3, double-blind, randomised, parallel-group trials. Lancet
Gastroenterol Hepatol. 2017;2(8):555-564.
Change from